Most Vulnerable More Likely to Depend on Emergency Rooms for Preventable Care
People in vulnerable populations — as defined by socioeconomic characteristics — made more preventable visits to emergency rooms than others from 2013 to 2017, according to a U.S. Census Bureau working paper.
The study analyzed census data linked with emergency visit records in the state of Utah. It found that factors including lower income, educational attainment, unemployment, lack of health insurance, lack of access to a vehicle or internet service were associated with a greater number of preventable visits.
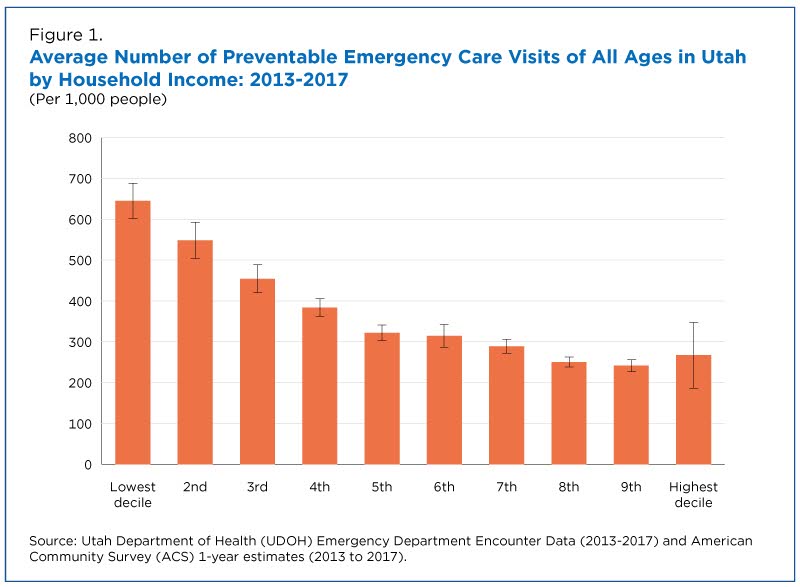
There was a clear correlation between income level and the frequency of preventable emergency care visits.
Visits to emergency departments are considered preventable when they are for health conditions that could have been handled in a non-emergency setting or avoided if the patient had adequate prior preventive care.
Among factors affecting the rate of preventable emergency room (ER) visits:
- Income.
- Education.
- Employment.
- Health insurance coverage.
- Transportation access.
- Internet access.
Using emergency rooms for preventable care may generate excess costs for taxpayers, increase provider burden, and reduce the quality of patient care.
Emergency department visits (both preventable and non-preventable) cost $76.3 billion in the United States in 2017, according to a study conducted by the U.S. Agency for Healthcare Research and Quality.
It is hard to quantify the savings but according to another national study published in Health Affairs, diverting preventable visits into other, more appropriate forms of care (i.e., urgent care clinics or retail clinics) may save an estimated $4.4 billion annually.
A Ground-Breaking Partnership
Despite the potential for savings and improvements in quality of care, there has not been much research evaluating the individual-level characteristics associated with preventable emergency department use due to data limitations.
With this study, researchers were able to link emergency department visits to socio-economic characteristics from the American Community Survey (ACS) due to a unique partnership between the Census Bureau and the Utah Department of Health (UDOH).
Using linked records, the researchers assessed patterns in preventable visits to emergency departments across Utah hospitals from 2013-2017. The linked data were then used to examine the social, demographic and economic factors that contributed to the rate of these visits.
Income and Education
There was a clear correlation between income level and the frequency of preventable emergency care visits.
Individuals in lower-income households, on average, visited emergency rooms for preventable reasons roughly 2.5 times as often as those with higher incomes (Figure 1).
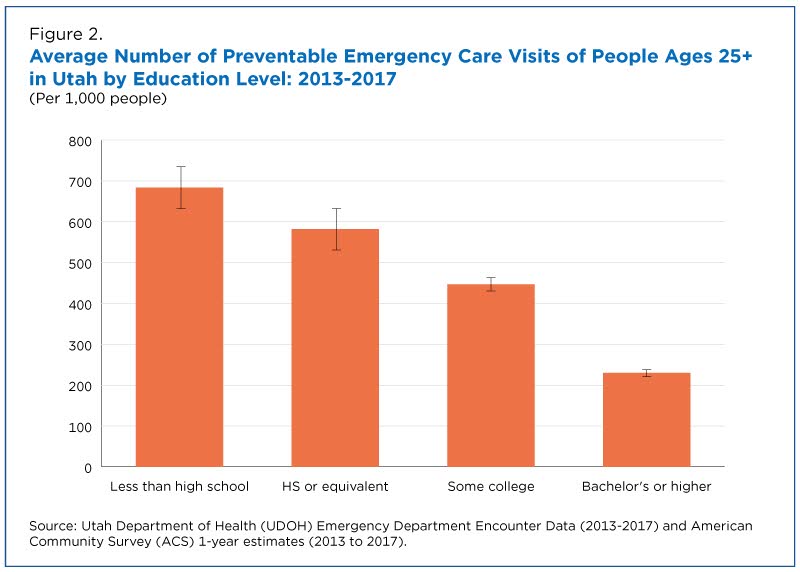
According to the study, individuals with lower educational attainment made more preventable emergency care visits than their more educated counterparts (Figure 2), likely because educational attainment is often linked with income and other socio-economic characteristics.
Individuals with less than a high school diploma made about three times as many preventable emergency care visits as those with a bachelor’s or higher degree.
Employment and Health Insurance
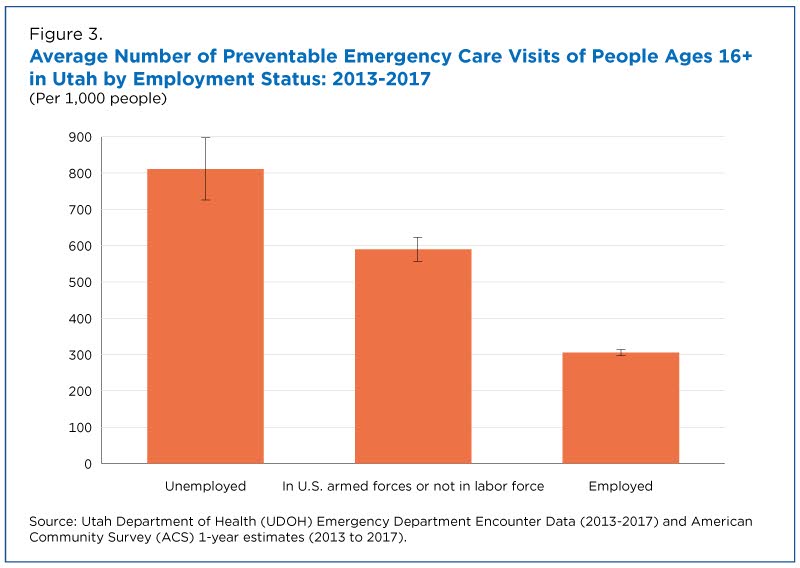
Individuals who were unemployed made roughly 2.5 times as many preventable emergency care visits as those who had a job (Figure 3).
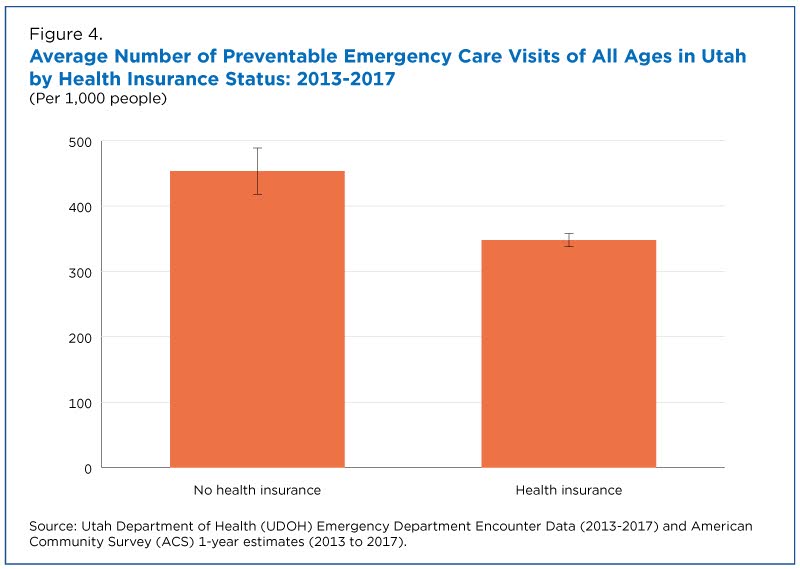
Lack of health insurance coverage was another factor that appeared to play a role in preventable ER visits.
According to the study, individuals without health insurance had more preventable visits to the ER than those with health insurance (Figure 4).
This suggests that uninsured individuals may not seek primary care for chronic conditions ahead of an urgent episode or they may rely on emergency rooms for general health care needs.
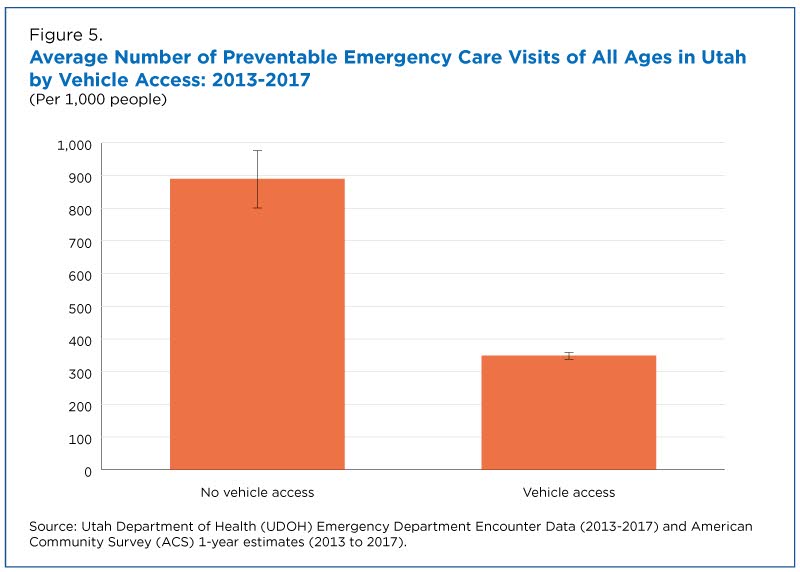
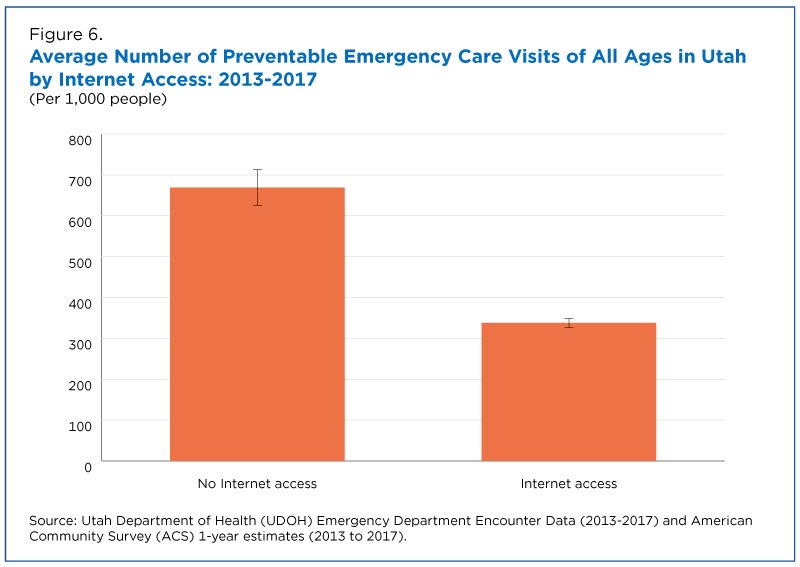
Access to Transportation and Internet
Lack of transportation and access to the Internet may also affect one’s ability to obtain health care.
The study showed that those without access to a vehicle had approximately 2.5 times as many ER visits as those with vehicle access (Figure 5).
Internet access may also play a role by limiting health care search options.
According to the study, people in households without internet access had twice as many preventable emergency care visits as those in households with internet access (Figure 6).
Potential for Innovative Partnerships and Data Linkages
For this study, researchers linked records of Utah emergency department visits and Census Bureau survey data at the individual level.
The researchers did not have access to personally identifiable information. The linked data could only be used by a limited number of researchers for statistical purposes.
In addition, the Census Bureau’s Disclosure Review Board reviewed all output for unauthorized disclosure of confidential information, and only approved aggregated output for release after applying disclosure avoidance rules.
The findings cited above are based on analyses of characteristics studied independently of one another. However, additional analyses looking at multiple factors at once are discussed in the paper.
The partnership between the Census Bureau and Utah Department of Health highlights that linking records using secure, anonymized methods can enhance patient health information with additional social determinants of health.
Additionally, this study met all of UDOH’s required Data Suppression and Data Aggregation Guidelines.
The COVID-19 pandemic has revealed important data gaps which may be filled using these types of record linkages.
The findings may help inform public health strategies and policies aimed at reducing preventable emergency care visits and healthcare costs.
This study was conducted by members of the Census Bureau’s Enhancing Health Data (EHealth) research program, which identifies opportunities to amplify health records with existing census data that health records commonly lack.
Through external partnerships, the EHealth team links together multiple data sources to create new data products on patient and provider characteristics, and it conducts research to help understand and advance population health.
Additional Resources
Please see the related interactive tool, Exploring Emergency Care in Utah, for more information about preventable emergency care in Utah.
Note: Select the image to go to the interactive data visualization.
Subscribe
Our email newsletter is sent out on the day we publish a story. Get an alert directly in your inbox to read, share and blog about our newest stories.
Contact our Public Information Office for media inquiries or interviews.
-
America Counts StoryWho Are Our Health Care Workers?April 05, 2021Health care, the nation’s largest and fastest-growing sector, employs 22 million. We profile this workforce now on the front line of the fight against COVID-19.
-
America Counts StoryPandemic Disrupts Some Trends in Health Care ServicesSeptember 08, 2021Estimates from the Quarterly Services Survey show that revenue percentage change for health care industries varied widely during the pandemic.
-
America Counts StoryWho Had Medical Debt in the United States?April 07, 2021Detailed tables from the Census Bureau’s Survey of Income and Program Participation provide a snapshot of households more likely to have medical debt in 2017.
-
Business and EconomyEconomic Census Geographic Area Statistics Data Now AvailableApril 07, 2025A new data visualization based on the 2022 Economic Census shows the changing business landscape of 19 economic sectors across the United States.
-
Income and PovertyWhat Sources of Income Do People Rely On?April 02, 2025A new interactive data tool shows income sources for hundreds of demographic and economic characteristic combinations.
-
Business and EconomyBig Improvements to the Annual Integrated Economic Survey (AIES)March 26, 2025The Census Bureau is making several changes and enhancements to capture 2024 economic data based on feedback from last year’s survey.
-
PopulationOnly 50 U.S. Counties Had Populations Over a Million in 2024March 17, 2025A new data visualization highlights U.S. counties between 1970 and 2024 whose populations ever surpassed a million.